BLUE LIGHT AGAINST ATOPIC DERMATITIS: NEW DETAILS RELATED TO THE SKIN MICROBIOME

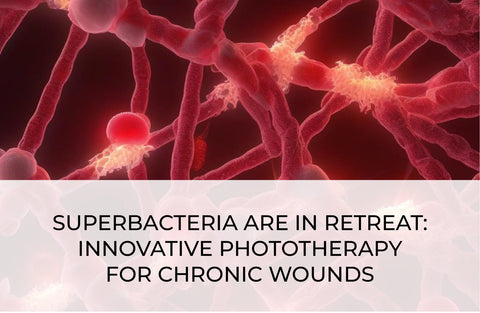
Atopic dermatitis (AD) is one of the most common chronic recurrent inflammatory skin diseases, affecting up to 3% of adults worldwide. The pathogenesis of AD is characterized by impaired epidermal barrier function and immune dysregulation. One of the causes of such disorders may be an increase in the number of S. aureus. This pathogen actively colonizes the skin of AD patients [1].
More and more scientific publications are devoted to evaluating the effectiveness of visible near-infrared light in treating AD. Blue light has attracted considerable attention due to its ability to modulate dendritic cell activation, positively influencing cell proliferation and inflammatory response in vitro.
In vivo studies have shown that whole-body irradiation with blue light (400–500 nm) reduces pruritus, improves quality of life, and reduces hydrocortisone use [2]. Likely, one of the ‘levers’ of the beneficial effects of blue light on atopic skin is the skin microbiome.
Staphylococcus aureus is present in increased numbers in AD rash foci. It can influence dendritic cell activation and itch severity through the induction of IL-31, which ultimately contributes to skin barrier disruption. Staphylococcus aureus has a golden yellow color due to the content of the carotenoid pigment staphyloxanthin, which shows characteristic absorption peaks at 408 nm and 486 nm [3].
The expression of this pigment promotes the survival of bacteria. Under conditions of oxidative stress, staphyloxanthin acts as an antioxidant that scavenges free radicals, thus enhancing the survival of Staphylococcus aureus both in vitroand in vivo in mouse models of chronic wounds [4].
The defense against free radicals through carotenoid expression is not unique to S. aureus. For example, the expression of carotenoid pigment is also characteristic of such skin commensals as M. luteus, Kocuria spp., and D.nishinomiyaensis [5]. The skin commensal M. luteus, which has probiotic properties, is highly resistant to UV light due to carotenoid expression, but the response to blue light remains to be evaluated. All these data suggest the microbiome's involvement in the mechanism of action of blue light on the skin of atopic patients. It means blue light represents a promising, non-invasive, non-medication approach to treating this chronic dermatosis. We are waiting for new clinical studies that will allow us to develop protocols for therapeutic and prophylactic photo procedures in this category of patients.
References
- Weidinger S., Beck L.A., Bieber T., Kabashima K., Irvine A.D. Atopic dermatitis. Nat Rev Dis Primers 2018; 4: 1.
- Uzunbajakava N.E., Tobin D. J., Botchkareva N.V., et al. Highlighting nuances of blue light phototherapy: Mechanisms and safety considerations. J. Biophotonics 2023; 16: e202200257.
- Harris D.M. Spectra of pathogens predict lethality of blue light photo-inactivation. Laser Ther 2023; 30.
- Campbell P.D., Miller A. M., Woesner M. E. Bright light therapy: seasonal affective disorder and beyond. Einstein J Biol Med 2017; 32: E13–e25.
- Koshti R., Jagtap A., Noronha D., et al. Evaluation of antioxidant potential and UV protective properties of four bacterial pigments. Microbiol Biotechnol Letters 2022; 50: 375–386.